Adhesive Capsulitis
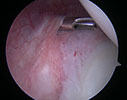
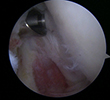
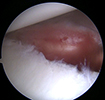
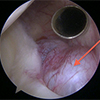
The patient is a 50 year-old female with Adhesive Capsulitis. Although her initial pain dissipated, she continued to suffer from a significant decrease in range of motion. After two years of symptoms, she decided to undergo an arthroscopic 360 degree capsular release. A combination of arthroscopic biters and shavers are used to release the capsule, but avoid injuring the underlying rotator cuff muscle and neurovascular structures (photo 1). The capsule should only be 1-2 mm in width, but with adhesive capsulitis the capsule can be up to 10 mm thick. At the time of surgery, her anterior and posterior capsule appeared thickened and stiff (photos 2,4). After surgery, the anterior and posterior capsule has been released (photos 3,5) and a normal range of motion has been restored. She went on to have full range of motion, was able to perform all of her activities of daily living, and returned to yoga and all of her sport activities.
Gird Release
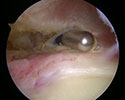
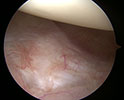
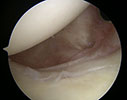
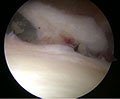
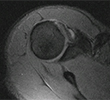
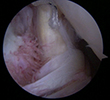
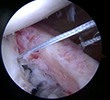
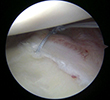
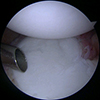
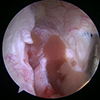
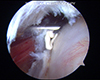
The patient is an elite level pitcher with decreased internal rotation, posterior labral fraying, and infraspinatus rotator cuff symptoms. His posterior labrum has become calcified on xrays and he has non-displaced posterior labral tearing on MRA. He has failed physical therapy and continued posterior impingement symptoms with throwing/pitching. At the time of shoulder arthroscopy, his posterior labrum was frayed (photo 1) and this was debrided. The undersurface of his infraspinatus is inflamed but not torn (photo 2). The posterior capsule is inflamed, stiff, and thickened (photo 3). The posterior capsule is released with the use of an arthroscopic scissors (photo 4). After release, the patients range of motion returned to that of the other side. He returned to pitching and went on to enter the MLB Draft.
Subscapularis Rotator Cuff Repair
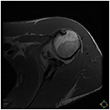
The patient is a 55 year old swimmer with persistent pain while swimming. His MRI (photo1) shows upper border tearing of the subscapularis. After failing conservative therapy, patient is taken to the operating room for an arthroscopic repair. During the arthroscopy (photo2), the subscapularis tendon is frayed and had a longitudinal split through the tendon. The tendon is debrided and an anchor is placed into the bone in the footprint of the sunscapularis attachment (photo3). The anchor is absorbable and will turn to bone over time. Stiches from the anchor are passed through the tendon and the tendon is tied or anchored down to the bone (photo4). The final repair demonstrates that the normal tubular appearance of the tendon and the normal tension has been restored. (photo 5)
Anterior Labral Repair for Glenohumeral Instability
The patient is a High School Pitcher who dislocated his throwing shoulder. Since it is his throwing shoulder, he elected to undergo surgical fixation of his labral lesion. Photos 1,2,3 demonstrate the torn anterior inferior labrum and its preparation to fixate the labrum and its attached ligaments back to bone. Photo 4 shows the hill sachs lesion (hole in the humeral head from the previous dislocation) which is engaging the glenoid (socket). Photos 5 and 6 demonstrate the labrum being repaired back to bone with suture anchors. After the repair, the ball is now sitting central in the socket (photo7). Restoration of the labrum and the capsulolabral complex results in moving the hill sachs lesion away from the glenoid. The patient returned to pitching and has earned a college scholarship.
Paralabral Cyst
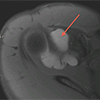
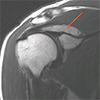
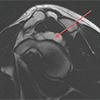
The patient is a world class triathlete who noticed increasing pain with overhead activities and swimming. The MRI images show a very large paralabral cyst which compresses the suprascapular nerve and displaces the supraspinatus muscle resulting in pain (photos 1,2,3,4 – cyst is shown by the arrows). During surgery the cyst is readily identified, opened and evacuated (photos 5,6,7). The abnormal tissue is debrided and the posterior capsule is released to prevent recurrence (photos 8,9). The patient has returned to winning triathalon competitions.
Little Leaguer's Shoulder
This 13 year old patient presented with a 2 month history of shoulder pain. On exam, the patient had a markedly diminished range of motion of the shoulder. The patient had been playing year round baseball since age 10 and pitches year round. X rays of his Left throwing shoulder (photo1,2,3) reveal a markedly widened growth plate from the repetitive stress of pitching and a low amount of time to heal. His right shoulder (photo 4) demonstrates what a normal proximal humeral growth plate should look like. After 3 months of rest and physical therapy to restore the normal motion of the shoulder, his growth plate has returned to a more normal appearance (photo 5) and he has gone on to safely return to pitching.
Latarjet
The Patient is an 18-year-old high level football player, who had his first shoulder dislocation when he was a freshman and became recurrently unstable during his junior year. At the time, he had a large fragment of bone and an arthroscopic boney Bankart repair was performed. The patient did well intially, but during his return to football broke apart the Bankart repair. He subsequently had recurrent episodes of dislocations throughout the season. The patient and his family elected patient elected to udergo left shoulder open capsulolabral repair and coracoid transfer. This is also known as Latarjet procedure. A latarjet procedure uses the bone of the coracoids to fill or augment the defect in the gleniod (socket of the shoulder). It is held in place with two lag screws
Chronic fiberous non union of old boney Bankart lesion from his first dislocation
MRI after the reinjury of boney Bankart repair with a large displaced boney lesion
Postoperative x-rays after Latarjet procedure
- Picture 1
- Picture 2
- Picture 3
- Picture 4
- Picture 5
- Picture 6
The patient is a 40 year old male with a large area of calcific tendonitis involving the anterior, inferior portion of his subscapularis tendon. The calcification was over 2 cm in size and would cause an audible snap as it popped across the conjoint tendon. Picture A shows the calcification and Picture B shows the calcium deposit being lanced with a spinal needle. Video clip #1 demonstrates the extraction of the calcium. Picture C and video clip #2 demonstrate the removal of all of the calcium. The patient returned to play without difficulty at 8 weeks.
Extraction of the calcium
Humeral and Glenoid Chondral Defects
These pictures demonstrate damage to the cartilage in a shoulder of a high level gymnast.
Arthroscopic Subacromial Decompression
Arthroscopic Debridement of Calcific Tendonitis
How is shoulder arthroscopy different than other surgeries?
Shoulder arthroscopy is a technique that has evolved in the United States over the last 25 years. Shoulder arthroscopy is technically demanding and is performed for treatment of labral lesions and rotator cuff tears. The patient is placed on their side and multiple portals are created to see and work within the shoulder joint and in the subacromial space. Dr Shepard trained in shoulder arthroscopy with world famous James R Andrews MD – one of the developers of the technique in the United States. Dr Andrews was the first to describe superior labral tears in high level baseball players. Dr Shepard regularly performs shoulder arthroscopy on people from high level athletes to non athletes.
Who needs shoulder arthroscopy?
There are two primary groups of people who undergo shoulder arthroscopy – young overhead athletes with labral tears from dislocations, SLAP tears, loose bodies; older people with rotator cuff tears.
The young athletes often develop SLAP lesions from repetitive overhead activities and labral tears / loose bodies from dislocations. These lesions can be treated through the arthroscope with loose body removal and labral repair. Sometimes, a capsular placation is performed to “tighten up” the capsule and ligaments of the shoulder. These injuries are most commonly seen in overhead athletes – swimmers, throwers, volleyball players, and water polo players, as well as young athletes who compete in contact sports that can often lead to dislocations – football, hockey, gymnastics, wrestling, and lacrosse.
The older person who tears his/her rotator cuff can be treated through the arthroscope as well. Most rotator cuff repairs that Dr Shepard performs are done through 3 or 4 portals (poke holes), rather than through a large, painful incision. The rotator cuff tendon can be repaired back to its anatomic location with the use of anchors (dry wall screws) and high strength sutures.